A Needs Assessment of Community Health Workers Who Work with Underserved Children and Families in the United States
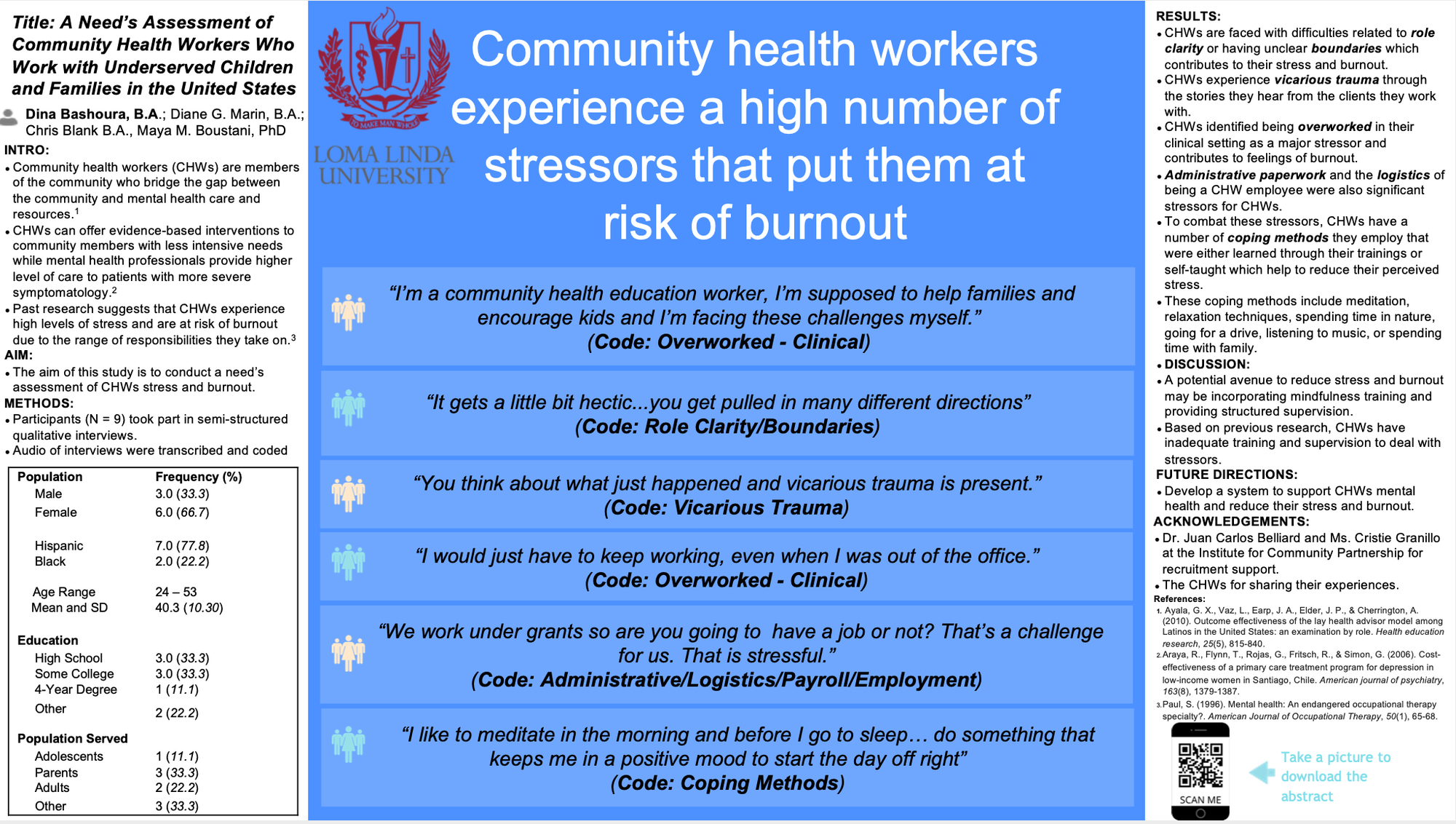
As a strategy to reduce the global prevalence of mental disorders, community health workers (CHWs) have been trained to deliver evidence-based treatments (EBTs) to underserved communities (Barnett et al., 2018). As members of the communities they serve, CHWs bridge the gap between community and care providers, build trust, address barriers to seeking care, reduce the stigma associated with receiving mental health care, and in turn, increase service engagement (Ayala et al., 2010). Furthermore, CHWs can offer case management and promotion of patient adherence to treatment and supply lower levels of care to patients with less intensive needs, while mental health professionals provide a higher level of care to patients with more severe symptomology (Araya et al., 2006). Because of the range of responsibilities CHWs take on, role blurring is a significant risk of working in community mental health (Paul, 1996). Past research suggests that the most stressful aspects of the CHWs job is increases in workload, time management, inappropriate referrals, role conflict, and a lack of supervision (Edwards et. al., 2000). According to Rhodes, the level of training and support that CHWs must receive to effectively carry out their role has not been established, though limited data suggests that ongoing supervision is needed (Rhodes et al. 2007). Data suggests that clarifying CHWs role in intervention delivery, the types of interventions they deliver, and the implementation support they receive is critical (Barnett et al., 2018). The aim of this project is to conduct a needs assessment of nine CHWs, recruited from the Institute for Community Partnership, through semi-structured qualitative interviews. The interviews cover a range of topics including current levels of stress and burnout as well as coping strategies to deal with that stress and burnout. Audio of interviews were transcribed and coded. Preliminary findings indicate that CHWs experience a high number of stressors that put them at risk of burnout. CHWs are faced with difficulties related to role clarity or having unclear boundaries which contributes to their stress and burnout. Additionally, CHWs experience vicarious trauma through the stories they hear from the clients they work with. CHWs identified being overworked in their clinical setting as a major stressor and contributes to feelings of burnout. Administrative paperwork and the logistics of being a CHW employee also showed to be a significant stressor for CHWs. CHWs acknowledge stressors other than the ones identified above that may play a role in burnout. To combat these stressors, CHWs have a number of coping methods they employ that were either learned through their trainings or self-taught which help to reduce their perceived stress. Future directions include developing a system to support CHWs mental health and reduce their stress and burnout.
References:
Araya, R., Flynn, T., Rojas, G., Fritsch, R., & Simon, G. (2006). Cost-effectiveness of a primary care treatment program for depression in low-income women in Santiago, Chile. American journal of psychiatry, 163(8), 1379-1387.
Ayala, G. X., Vaz, L., Earp, J. A., Elder, J. P., & Cherrington, A. (2010). Outcome effectiveness of the lay health advisor model among Latinos in the United States: an examination by role. Health education research, 25(5), 815-840.
Barnett, M. L., Gonzalez, A., Miranda, J., Chavira, D. A., & Lau, A. S. (2018). Mobilizing community health workers to address mental health disparities for underserved populations: A systematic review. Administration and Policy in Mental Health and Mental Health Services Research, 45(2), 195-211.
Edwards, D., Burnard, P., Coyle, D., Fothergill, A., & Hannigan, B. (2000). Stress and burnout in community mental health nursing: a review of the literature. Journal of psychiatric and mental health nursing, 7(1), 7-14.
Paul, S. (1996). Mental health: An endangered occupational therapy specialty?. American Journal of Occupational Therapy, 50(1), 65-68.
Rhodes, S. D., Foley, K. L., Zometa, C. S., & Bloom, F. R. (2007). Lay health advisor interventions among Hispanics/Latinos: a qualitative systematic review. American journal of preventive medicine, 33(5), 418-427.